Schizophrenia
Our research is focused on understanding the underlying causes of schizophrenia and finding new treatments that not only improve symptoms but ultimately, improve quality of life for people affected.
Our research is focused on understanding the underlying causes of schizophrenia and finding new treatments that not only improve symptoms but ultimately, improve quality of life for people affected.

Outward symptoms of schizophrenia usually become evident in adolescence or young adulthood. Women tend to have a slightly later age of onset.
A person with schizophrenia may initially appear withdrawn or depressed and later on express unusual thoughts or beliefs. At first, they are typically not aware of their symptoms and they do not understand that they are unwell.
Symptoms can be divided into two categories: positive symptoms (behaviour or feelings that people with schizophrenia experience but are not commonly observed in healthy people) and negative symptoms (behaviour or feelings that are missing in people with schizophrenia but are commonly observed in healthy people).
Positive symptoms include auditory hallucinations and delusions. Auditory hallucinations often take the form of one or more voices, perceived by the person with schizophrenia as someone speaking out loud. These voices often comment on the persons behaviour and are often experienced as someone saying mean things about the person with schizophrenia.
Negative symptoms include a lack of emotion and motivation, minimal speech and deficits in the ability to think clearly.
Schizophrenia can appear to be somewhat different in different people. Some people experience more hallucinations and delusions, while others primarily experience disordered thoughts and speech. Some people also experience depression and mania (symptoms seen in people with bipolar disorder) which is characteristic of schizoaffective disorder.
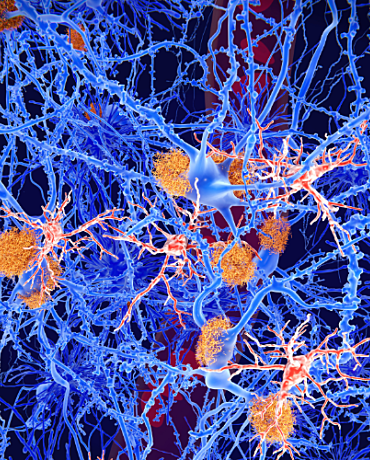
Researchers have found a handful of genes that may be linked to schizophrenia. Some of these genes relate to a neurotransmitter called glutamate, which plays a major role in brain development. Its been suggested that the glutamate system may not function properly in people with schizophrenia. Other candidate genes relate to another neurotransmitter called dopamine. Its also been shown that the dopamine system does not function properly in the brains of people with schizophrenia.
At NeuRA, researchers have discovered that people with schizophrenia are more likely to inherit a gene that codes for a faulty oestrogen receptor in the brain. We are continuing to look at how genes and environmental factors cause schizophrenia in the brain during development.
A more complete knowledge of these causes could lead to new and more effective treatments for schizophrenia. Identifying and testing these potential treatments in clinical trials could reduce symptoms, improve thinking, restore normal social function and improve quality of life for sufferers.
Antipsychotic medication may reduce some symptoms but does not return people to their pre-illness level of function. We have discovered that some people with schizophrenia have a gene that does not allow the brain to respond to hormones.
Based on this finding, we have started to test a new treatment that can stimulate the hormonal receptors in the brain. This improves brain activity, learning, memory and attention.
These topics cover symptoms, treatments, diagnosis, risk factors, outcomes, co-occurring or comorbid conditions, epidemiology (population perspectives), and the physical features of schizophrenia. This evidence, all derived from systematic reviews is summarised and quality assessed so that the strength of the evidence can be measured.
Every dollar of community support enables our scientists to continue making life-changing discoveries that contribute to a brighter and healthier future.
Run, swim or bake your way to making a positive difference in the lives of people touched by brain and nervous system disorders.
Stay informed about our latest research breakthroughs, scientific discoveries and the incredible minds behind them – subscribe today.
Neuroscience Research Australia respectfully acknowledges the Bidjigal and Gadigal peoples of the Eora Nation as the Traditional Owners of the Land on which we stand and pay our respects to Elders past and present.
Redevelopment of the NeuRA website has been made possible by the generous support of Conexus Financial.