Sleep apnoea
Sleep apnoea is one of the most common sleep disorders, affecting approximately 5% of the Australian population. Our goal is to find better ways to treat sleep apnoea and improve health outcomes for individuals affected.
Sleep apnoea is one of the most common sleep disorders, affecting approximately 5% of the Australian population. Our goal is to find better ways to treat sleep apnoea and improve health outcomes for individuals affected.
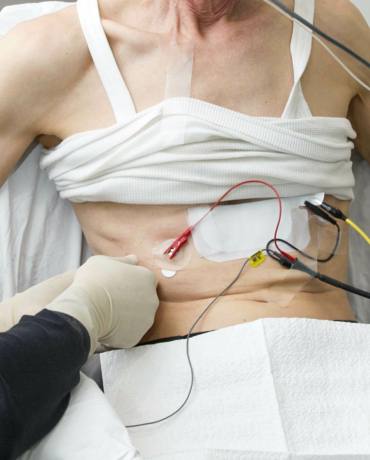
NeuRA is currently making the first direct biomechanical measurements of the upper airway in humans, an area of the body thought to be key to how sleep apnoea operates. By examining how the brain drives these muscles and the change in their function due to obstructive sleep apnoea, we will be able to improve treatments.
While continuous positive airway pressure (CPAP) is highly effective in treating sleep apnoea, it does not work for approximately 50% of patients. NeuRA’s goal in this area is to develop accurate tools to identify the varying causes of sleep apnoea, develop targeted novel therapies for individual patients, and to determine who is most likely to respond to existing non-CPAP therapies.
Much of our research focuses on the upper airways including where we are measuring the stiffness of the muscles and how they move during normal breathing. The aim is to understand what predisposes them to collapse. We are also measuring the electrical signals from the brain to the major muscle, the genioglossus, to understand how it contracts to keep the upper airway open.
Medication also has an impact so we are looking at sleeping pills and opioids. Approximately 5% of adults report using sleeping pills to promote sleep, with higher rates in the elderly. Our researchers are conducting studies of healthy individuals and sleep apnoea patients to examine the effects of sleeping pills on the upper airway muscles and breathing during sleep.
In terms of opioids, we are investigating the effects on upper airway muscle activity, respiratory control, and breathing during sleep in patients with obstructive sleep apnoea. This research will help us understand why breathing responses to opioids vary between individuals and which sleep apnoea patients are most at risk of developing breathing complications.
NeuRA has found that the motion of the genioglossus muscle connected to the tongue is significantly different in sleep apnoea patients compared to healthy research participants. It also varies with the severity of the disease. As the disease develops, tongue motion increases, but is not well coordinated. This means that instead of opening the airway, contraction can widen one region and narrow another. In the most severe cases, motion appears to reduce or cease so that the genioglossus does not dilate the airway during each breath.
We are now in a unique position to visualise how the brain communicates via the electrical signals with muscles in the upper airway. This will provide critical information about how the upper airway works normally and how its function is impaired in obstructive sleep apnoea.

Senior Principal Research Scientist
Every dollar of community support enables our scientists to continue making life-changing discoveries that contribute to a brighter and healthier future.
Run, swim or bake your way to making a positive difference in the lives of people touched by brain and nervous system disorders.
Stay informed about our latest research breakthroughs, scientific discoveries and the incredible minds behind them – subscribe today.
Redevelopment of the NeuRA website has been made possible by the generous support of Conexus Financial.
Neuroscience Research Australia respectfully acknowledges the Bidjigal and Gadigal peoples of the Eora Nation as the Traditional Owners of the Land on which we stand and pay our respects to Elders past, present and future.