Research Project

Siobhan Schabrun
Current Appointments
Senior Research Scientist and Group Leader, NeuRAKey Research Areas
Dr Siobhan Schabrun trained as a physiotherapist before completing a PhD in neuroscience at The University of Adelaide in 2009. Supported by a NHMRC Early Career Fellowship, she undertook post-doctoral training in pain neuroscience at The University of Queensland. In 2014, she received a Fulbright scholarship to further her interest in the neuroplasticity of pain in the USA and was awarded a QLD Young Tall Poppy Science Award. In 2018 she moved to NeuRA where she leads a program of research that seeks to understand why some people recover after an episode of musculoskeletal pain while others develop long-lasting, disabling pain. She is the 2020 Ulf Lindblom Award Recipient for an outstanding young clinical investigator in the field of pain.
Research interests include the discovery of biomarkers that can predict who will develop chronic pain – even before pain begins, investigation of the neurobiological mechanisms that underpin the transition from acute to chronic pain and the development and testing of non-invasive brain stimulation treatments for chronic pain. She is also passionate about improving the translation of research evidence into clinical practice. Follow Siobhan’s work on Google Scholar.
Siobhan is deputy lead of the low back pain working group of the SPHERE musculoskeletal clinical academic group, a nominated member of the Global Young Academy and is one of the inaugural Superstars of STEM.
Publications
2023, 14 Dec
Phosphene and Motor Transcranial Magnetic Stimulation Thresholds Are Correlated: A Meta-Analytic Investigation
View full preprint on https://doi.org/10.1101/2023.12.12.571304
2023, 17 Nov
Effects of nicotine compared to placebo gum on sensitivity to pain and mediating effects of peak alpha frequency
View full preprint on https://doi.org/10.7554/eLife.91933.1
2023, 17 Nov
Effects of nicotine compared to placebo gum on sensitivity to pain and mediating effects of peak alpha frequency
View full preprint on https://doi.org/10.7554/eLife.91933
2023, 16 Nov
Can non-invasive brain stimulation modulate peak alpha frequency in the human brain? A systematic review and meta-analysis
View full preprint on https://doi.org/10.1101/2023.11.13.566909
2023, 14 Aug
Effects of nicotine compared to placebo gum on sensitivity to pain and mediating effects of peak alpha frequency
View full preprint on https://doi.org/10.1101/2023.08.11.552723
2023, 29 Jun
Systemic pro- and anti-inflammatory profiles in acute non-specific low back pain: An exploratory longitudinal study of the relationship to six-month outcome
View full journal-article on https://doi.org/10.1371/journal.pone.0287192
2023 Apr
Human assumed central sensitization in people with acute non‐specific low back pain: A cross‐sectional study of the association with brain‐derived neurotrophic factor, clinical, psychological and demographic factors
View full journal-article on https://doi.org/10.1002/ejp.2078
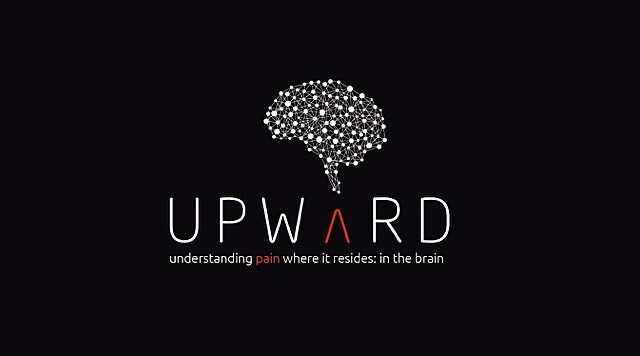
2023 Jan
Cortical function and sensorimotor plasticity are prognostic factors associated with future low back pain after an acute episode: the Understanding persistent Pain Where it ResiDes prospective cohort study
View full journal-article on https://doi.org/10.1097/j.pain.0000000000002684
2022 Oct
The Effect of Acute and Sustained Pain on Corticomotor Excitability: A Systematic Review and Meta-Analysis of Group and Individual Level Data
View full journal-article on https://doi.org/10.1016/j.jpain.2022.04.012
2022 Jul
Interhemispheric Inhibition Between Primary Sensory Cortices is not Influenced by Acute Muscle Pain
View full journal-article on https://doi.org/10.1016/j.jpain.2022.01.005