Research Project

Adam Walker
Current Appointments
Research Fellow, Group Leader - Laboratory of Immunopsychiatry, Neuroscience Research AustraliaKey Research Areas
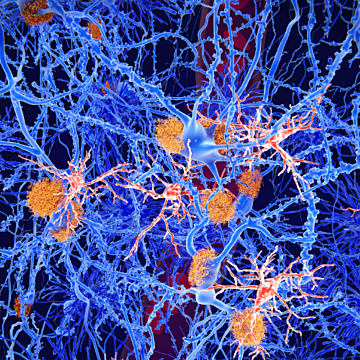
The Laboratory of ImmunoPsychiatry, led by Dr Adam Walker, investigates the role of the immune system and inflammation in symptoms of psychiatric illness. We investigate the mechanisms responsible for inflammation-associated psychiatric disorders such as depression and schizophrenia, neurodevelopmental disorders such as Tourette’s Syndrome and Autism, and when symptoms of depression and cognitive impairment occur in patients with chronic inflammatory illness such as cancer (known as ‘chemobrain’). The Laboratory of ImmunoPsychiatry is dedicated to identifying potential cheap available drugs that can be repurposed to prevent and treat psychiatric illness and to identify new biological targets for novel drug design.
Dr Adam Walker completed his PhD at the University of Newcastle in 2011 and completed successful postdoctoral fellowships at the University of Illinois – Urbana-Champaign and The University of Texas MD Anderson Cancer Center. He returned to Australia in 2015 and joined Monash University as a National Breast Cancer Foundation research fellow, investigating the mechanisms underlying cognitive and psychiatric side-effects of cancer and its treatment. Now at NeuRA, Adam’s research focuses on mechanisms of inflammation-induced depression, schizophrenia and cancer-associated cognitive impairment. He has pioneered discovery of available drugs that may be repurposed to prevent treat inflammation-induced depression (ketamine, leucine) and cancer-associated cognitive impairment (aspirin).
Publications
2024, 01 Dec
The search for gastrointestinal inflammation in autism: a systematic review and meta-analysis of non-invasive gastrointestinal markers
View full journal-article on https://app.dimensions.ai/details/publication/pub.1168010232
2024, 01 Jan
Immp2l Enhances the Structure and Function of Mitochondrial Gpd2 Dehydrogenase
View full journal-article on https://app.dimensions.ai/details/publication/pub.1167918317
2023, 01 Nov
Type of anesthesia for cancer resection surgery: No differential impact on cancer recurrence in mouse models of breast cancer
View full journal-article on https://app.dimensions.ai/details/publication/pub.1166403261
2023, 24 Aug
Immp2l knockdown in male mice increases stimulus-driven instrumental behaviour but does not alter goal-directed learning or neuron density in cortico-striatal circuits in a model of Tourette syndrome and autism spectrum disorder
View full journal-article on https://app.dimensions.ai/details/publication/pub.1162934469
2023 Aug
Antioxidant Behavioural Phenotype in the <i>Immp2l</i> Gene Knock-Out Mouse
View full journal-article on https://www.mdpi.com/2073-4425/14/9/1717
2023, 01 Jul
Changes in cytokine and cytokine receptor levels during postnatal development of the human dorsolateral prefrontal cortex
View full journal-article on https://app.dimensions.ai/details/publication/pub.1156378812
2023, 01 Jul
Increased prefrontal cortical cells positive for macrophage/microglial marker CD163 along blood vessels characterizes a neuropathology of neuroinflammatory schizophrenia
View full journal-article on https://app.dimensions.ai/details/publication/pub.1156492860
2023, 01 Apr
receiving endocrine therapy: what are the impacts?
View full journal-article on https://app.dimensions.ai/details/publication/pub.1156496810
2023, 01 Jan
Beta-blockade enhances anthracycline control of metastasis in triple-negative breast cancer
View full journal-article on https://app.dimensions.ai/details/publication/pub.1157546268
2022, 01 Dec
Cancer activates microglia to the same extent as chronic stress throughout stress neurocircuitry in a mouse model of breast cancer
View full journal-article on https://app.dimensions.ai/details/publication/pub.1151187166