Research Project

Bart Bolsterlee
Current Appointments
Senior Research FellowKey Research Areas
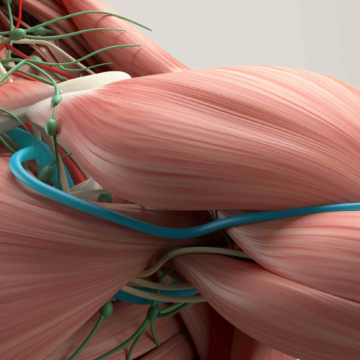
Dr Bart Bolsterlee is a mechanical engineer (BSc) and biomedical engineer (MSc, PhD) who studies the generation of force and movement in humans. His specialty is the use of imaging technologies such as MRI and ultrasound to study human movement biomechanics. In 2014 he completed his PhD in biomechanical modelling of the human upper limb at Delft University of Technology (The Netherlands). His current work at NeuRA focuses on the use of diffusion tensor imaging (DTI; an MRI technique) to measure muscle structure. He has recently developed novel algorithms to obtain quantitative measurements of muscle architecture by combining information from anatomical MRI and DTI scans. He applies these techniques to study mechanisms of muscle contracture (stiffening of muscles) in patients with stroke and cerebral palsy. He also performs studies in basic muscle physiology and biomechanics to elucidate the mechanical role of active and passive structures in muscles, and to study how muscles change shape following exercise.
Dr Bart Bolsterlee’s work has been published in high-quality journals such as Journal of Biomechanics, Journal of Applied Physiology and PlosONE. He is the secretary/treasurer of the Australian and New Zealand Society of Biomechanics.
Publications
2024 Jul
Hybrid dual mean-teacher network with double-uncertainty guidance for semi-supervised segmentation of magnetic resonance images
View full journal-article on http://dx.doi.org/10.1016/j.compmedimag.2024.102383
2023 Dec
Three-dimensional architecture of the human subscapularis muscle in vivo
View full journal-article on http://dx.doi.org/10.1016/j.jbiomech.2023.111854
2023, 06 Nov
Compositional and Functional MRI of Skeletal Muscle: A Review
View full journal-article on https://doi.org/10.1002/jmri.29091
2023, 02 Nov
Human lower leg muscles grow asynchronously
View full journal-article on http://dx.doi.org/10.1111/joa.13967
2023 Jul
Strain-dependent shear properties of human adipose tissue in vivo
View full journal-article on https://doi.org/10.1016/j.jmbbm.2023.105924
2023 Jun
Three-dimensional skeletal muscle architecture in the lower legs of living human infants
View full journal-article on http://dx.doi.org/10.1016/j.jbiomech.2023.111661
2023
Uncertainty and Shape-Aware Continual Test-Time Adaptation for Cross-Domain Segmentation of Medical Images
View full book-chapter on http://dx.doi.org/10.1007/978-3-031-43898-1_63
2022, 28 Mar
Hybrid Attentive Unet for Segmentation of Lower Leg Muscles and Bones From MRI Scans For Musculoskeletal Research
View full conference-paper on http://dx.doi.org/10.1109/isbi52829.2022.9761501
2022, 01 Mar
A new framework for analysis of three-dimensional shape and architecture of human skeletal muscles from in vivo imaging data
View full journal-article on https://doi.org/10.1152/japplphysiol.00638.2021
2022 Jan
Regional variation in lateral and medial gastrocnemius muscle fibre lengths obtained from diffusion tensor imaging
View full journal-article on https://doi.org/10.1111/joa.13539